整理撰文 / 張中維藥師
更新日期:2023/12/18
美國糖尿病協會(American Diabetes Association, ADA)於2023年12月11日更新了糖尿病臨床照護指引(Standards of Care in Diabetes—2024),本篇文章整理了這次修訂的內容,並提供最新的糖尿病治療指引準則,供醫療人員參考。內容若有疑義,還請不吝嗇提出指教!
2024版本全文下載連結:Standards of Care in Diabetes—2024
文章目錄
2024年ADA主要修訂內容
2024年糖尿病臨床照護指引中較大的更新包括:
- 糖尿病患者肥胖管理建議更新,包括減少治療惰性(therapeutic inertia)1、擬定個體化治療方案(personalization)以及針對BMI超標者制定測量標準(如:腰圍、腰臀比、腰高比)。
- 新增糖尿病患者心衰竭(heart failure)篩檢建議。
- 更新糖尿病患者周邊動脈疾病(peripheral arterial disease, PAD)篩檢建議。
- 新增teplizumab2的篩檢與使用指引。
- 更新glucagon-like peptide 1 (GLP-1) agonists與dual glucose-dependent insulinotropic polypeptide (GIP) receptor agonists用於減肥控制的指引,協助患者達到目標體重。
- 更新糖尿病指引中的診斷與分類。
- 強調低血糖的預防與管理。
- 強調在基層醫療院所篩檢糖尿病患者是否有非酒精性脂肪肝疾病(nonalcoholic fatty liver disease, NAFLD)與非酒精性脂肪肝炎(nonalcoholic steatohepatitis, NASH)。
- 加入評估糖尿病患者骨骼健康,並新增糖尿病患者骨折風險因子。
- 強調加強對失能(disability)糖尿病患者的篩檢與疾病管理。
- 強調醫療提供者應使用先進技術(如:人工智慧進行視網膜篩檢)與數位遠距醫療,加強對糖尿病患者的管理與教育。
- 新增新發行第一型糖尿病(new onset type 1 diabetes)與COVID-19感染之間的潛在關聯性。
- 治療惰性(therapeutic inertia):醫療機構為落實應該開始或是給予升階治療的處方。 ↩︎
- teplizumab(TzieldTM):2022年通過美國FDA核准,成為第一個用於延緩第一型糖尿病病程的藥物(FDA NEWS)。 ↩︎
第一章修訂內容(改善照護與促進健康)
- 新增2015年至2018年美國糖尿病患者的血脂、血壓、血糖數值控制現況(僅50.5%糖尿病成人A1C<7%;47.7%血壓<130/80 mmHg;55.7% non-HDL膽固醇<130 mg/dL)。
- 三家主要胰島素製造廠商降低胰島素價格,改善成本相關藥物不順從性(cost-related medication non-adherence)。
- 強調社區護理人員的重要性,可以提供慢性病監測、教育、藥物管理、傷口護理與急救服務。
第二章修訂內容(糖尿病的診斷與分類)
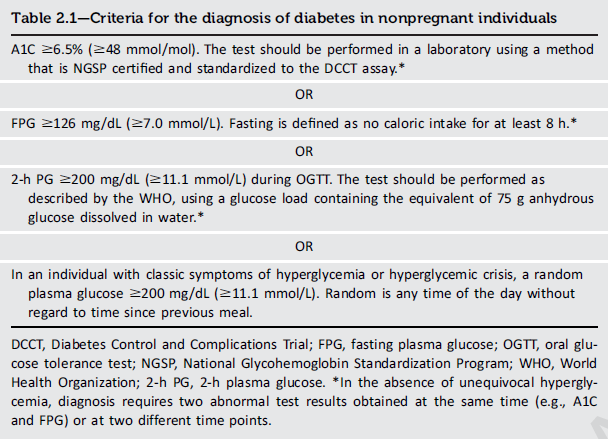
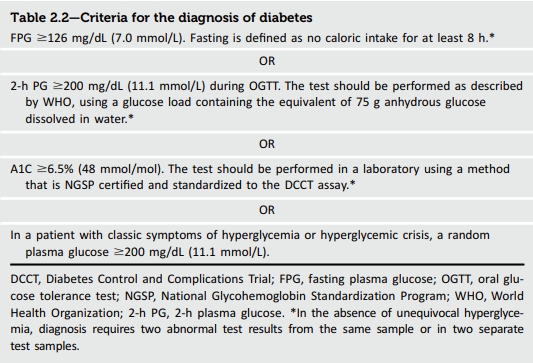
- 新版糖尿病診斷標準中將A1C挪至流程頂部,強調其對於糖尿病與糖尿病前期診斷的重要性。
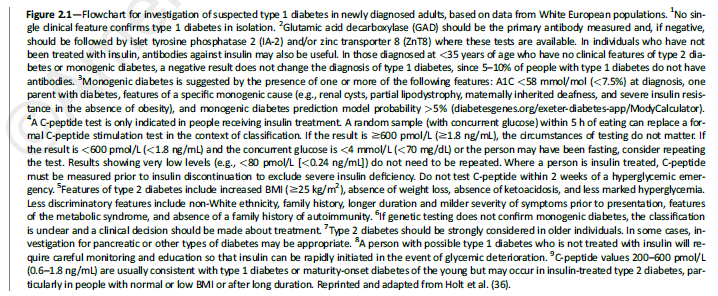
- 新增懷疑患有第1型糖尿病成年人的診斷流程。
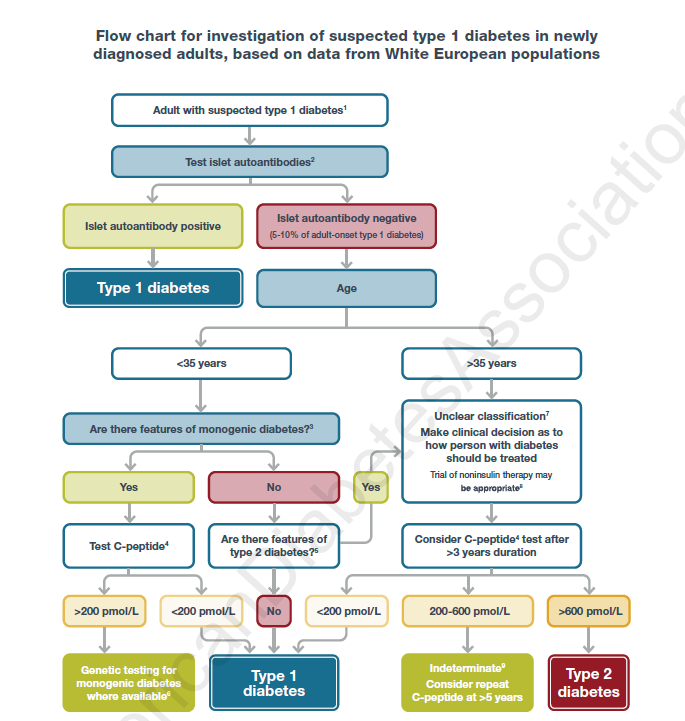
(圖片來源:ADA-Standards of Care in Diabetes—2024)
- 新增一段落描述COVID-19感染與新發第1型糖尿病之間可能存在關聯性。
A number of viruses have been associated with type 1 diabetes, including enteroviruses such as Coxsackievirus B. During the coronavirus disease 2019 (COVID-19) pandemic, cases of hyperglycemia, DKA, and new diabetes increased, suggesting that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a trigger for or can unmask type 1 diabetes. Possible mechanisms of β-cell damage include virus-triggered β-cell death, immune-mediated loss of pancreatic β-cells, and damage to β-cells because of infection of surrounding exocrine cells. The cytokine storm associated with COVID-19 infection is a highly inflammatory state that could also contribute. To better characterize and understand the pathogenesis of new-onset COVID-19–related diabetes, a global registry, CoviDIAB, has been established.
- 強調幾種藥物類別在增加糖尿病前期和2型糖尿病風險方面的作用,以及篩查的必要性。
Consider screening people for prediabetes or diabetes if on certain medications, such as glucocorticoids, statins, thiazide diuretics, some HIV medications, and second-generation antipsychotic medications, as these agents are known to increase the risk of these conditions.
- 強調在急性胰腺炎發作後或慢性胰腺炎患者中進行糖尿病篩查的重要性。
Screen people for diabetes within 3–6 months following an episode of acute pancreatitis and annually thereafter. Screening for diabetes is recommended annually for people with chronic pancreatitis.
第三章修訂內容(預防或延遲糖尿病及相關共病)
- 強調監測有發展第1型糖尿病風險個體的重要性。
In people with preclinical type 1 diabetes, monitor for disease progression using A1C approximately every 6 months and 75-g oral glucose tolerance test (i.e., fasting and 2-h plasma glucose) annually; modify frequency of monitoring based on individual risk assessment based on age, number and type of autoantibodies, and glycemic metrics.
- 增加了建議3.15,針對teplizumab使用進行討論,該藥物已被批准用於延遲成年人和8歲及以上兒童的三期第1型糖尿病發病。
Teplizumab-mzwv infusion to delay the onset of symptomatic type 1 diabetes (stage 3) should be considered in selected individuals aged ≥8 years with stage 2 type 1 diabetes. Management should be in a specialized setting with appropriately trained personnel.
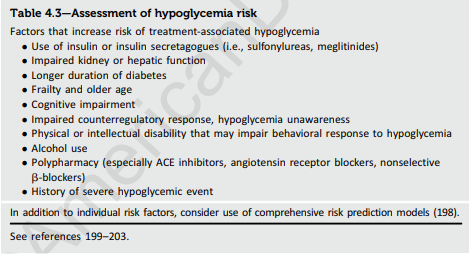
第四章修訂內容(全面醫學評估和共病評估)
- 更新了圖4.1,新增在選擇治療時考慮個人的生活方式選擇(lifestyle choices)。
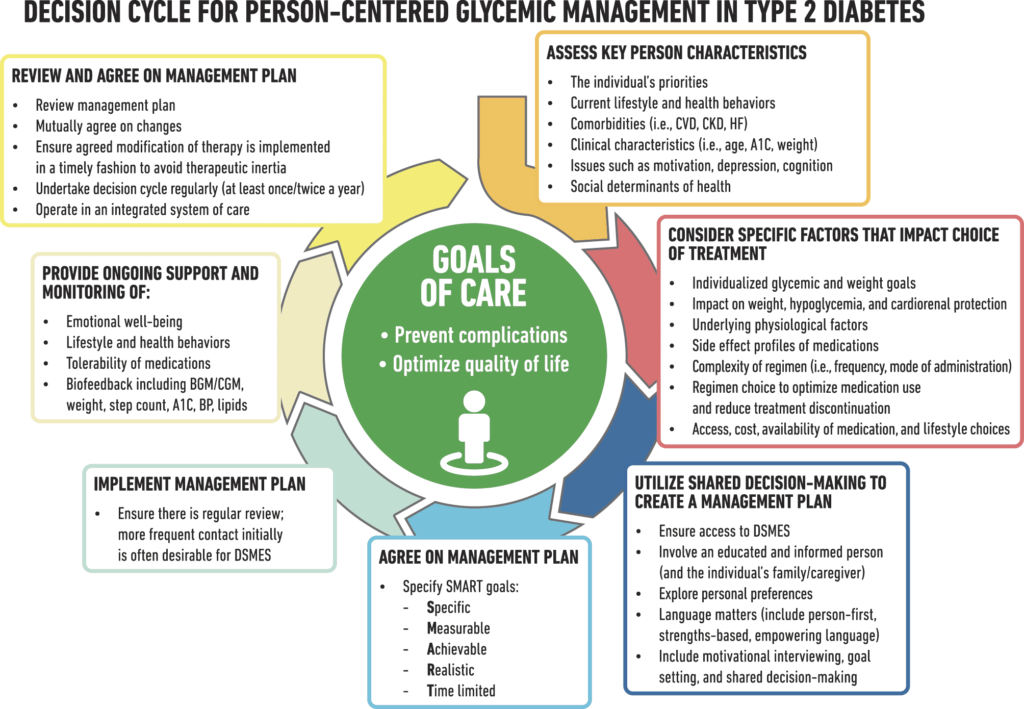
(圖片來源:ADA-Standards of Care in Diabetes—2024)
- 在預防接種小節中更新了有關60歲以上慢性病患者(如糖尿病)的COVID-19疫苗及呼吸道合胞病毒疫苗的信息。並移除2023版本表格中HPV疫苗接種建議。
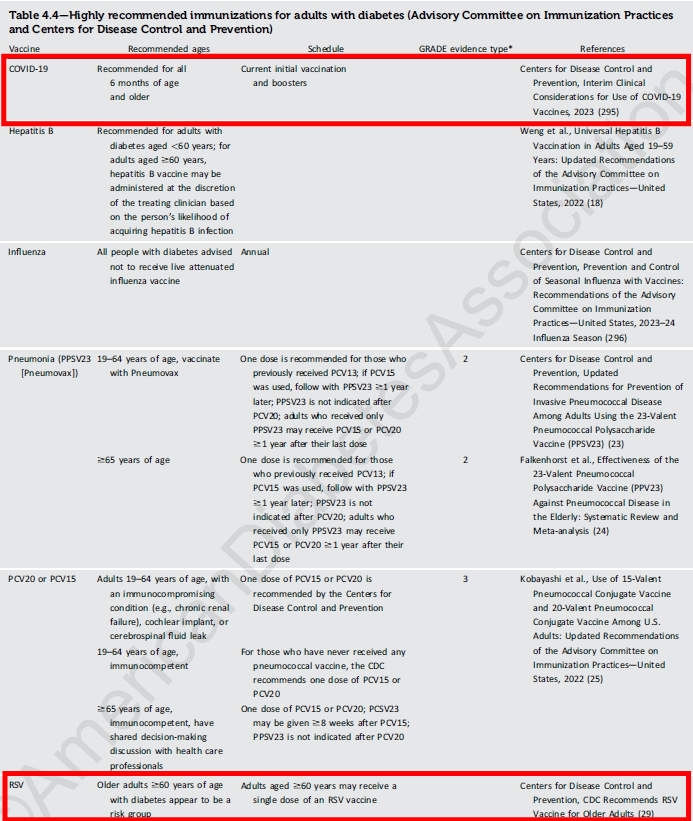
(圖片來源:ADA-Standards of Care in Diabetes—2024)
- 新增糖尿病與骨骼健康相關資訊。應每2-3年監測高風險的老年糖尿病患者(年齡>65歲)和年輕但具有多個危險因子糖尿病患者的骨礦物密度。
- 針對骨折風險較高的糖尿病患,優先使用與低血糖風險較低相關的降糖藥物,以避免跌倒。
- 新增骨折一般危險因子以及糖尿病患者額外的危險因子。
Monitor bone mineral density using dual-energy X-ray absorptiometry of high-risk older adults with diabetes (aged >65 years) and younger individuals with diabetes and multiple risk factors every 2–3 years.
To reduce the risk of falls and fractures, glycemic management goals should be individualized for people with diabetes at a higher risk of fracture. Prioritize use of glucose-lowering medications that are associated with low risk for hypoglycemia to avoid falls.
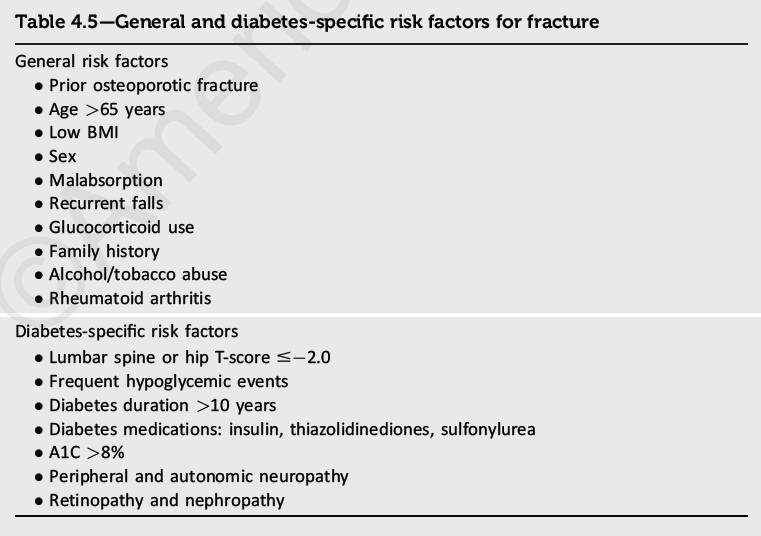
(圖片來源:ADA-Standards of Care in Diabetes—2024)
第五章修訂內容(促進積極的健康行為和福祉以改善健康成果)
第5節的重點放在指導醫療專業人員的行為上,而非糖尿病患者。
- 以人為中心的護理建議中,更廣泛地融合文化敏感性。增加有關宗教性禁食的小節,並介紹了時序營養學(飲食對生理時鐘影響)的概念。
| 主題 | 2024版本 | 2023版本 |
|---|---|---|
| 飲食模式與膳食規劃 | 討論了各種飲食模式,如地中海式、DASH、低碳水化合物素食和植物性飲食。強調對於糖尿病患者並無理想的碳水化合物、蛋白質和脂肪的卡路里比例,推崇根據個人飲食風格和目標進行個性化的膳食規劃。 | 與2024年版本相似。 |
| 飲食方法 | 提到不同的飲食方法,如盤餐法和碳水化合物計算,強調根據個人需求調整飲食。 | 並未詳細介紹具體飲食方法,但強調選擇整體食物而非高度加工食物,並個性化飲食模式。 |
| 飲食模式研究 | 討論了隨機對照試驗和系統評價等研究方法,強調各種飲食模式均可,但未推薦特定模式。 | 與2024年版本相似。 |
| 膳食規劃 | 強調營養師在創建個人化膳食計劃中的角色,並介紹不同的膳食規劃方法。 | 與2024年版本相似。 |
| 飲食方法/手段 | 比較了不同的飲食方法,如碳水化合物計數和盤餐法,引用研究證據。 | 討論了糖尿病盤餐法和碳水化合物計數,著重於其在改善A1C水平方面的有效性。 |
| 間歇性禁食與時間限制進食 | 詳述了各種間歇性禁食的形式及其對體重和血糖管理的影響。 | 與2024年版本相似。 |
| 碳水化合物 | 討論了對理想碳水化合物攝取量的研究結論不一,強調應選擇高質量的碳水化合物來源。 | 與2024年版本相似。 |
| 蛋白質 | 談及蛋白質攝取量、其在糖尿病管理中的作用以及相關健康風險。 | 與2024年版本相似。 |
| 脂肪 | 討論了飲食中脂肪的作用,強調脂肪類型比總量更重要。 | 與2024年版本相似。 |
| 鈉 | 建議糖尿病患者限制鈉攝取量,給出了一般建議。 | 同樣建議限制鈉攝取量,並考慮食物的可口性和營養充足性。 |
| 微量營養素和補充劑 | 討論了飲食補充劑的效益缺乏證據,並強調某些補充劑的潛在風險。 | 與2024年版本相似。 |
| 酒精 | 討論了糖尿病患者飲酒的風險和指南。 | 與2024年版本相似。 |
| 非營養性甜味劑 | 延伸探討非營養性甜味劑在糖尿病管理中的作用和安全性。 | 與2024年版本相似。 |
- 煙草、電子煙和大麻小節中新增「大麻」,以包括對大麻使用的討論。
Evidence of specific increased risk of diabetic ketoacidosis and hyperglycemic ketosis associated with cannabis use and cannabis hyperemesis syndrome in adults with type 1 diabetes has been recently reported.
第六章修訂內容(血糖目標和低血糖)
- 更新了建議6.1,包括對需要更密切血糖監測的人群進行更頻繁的血糖評估。
- 更新連續血糖監測(CGM)指標與目標。
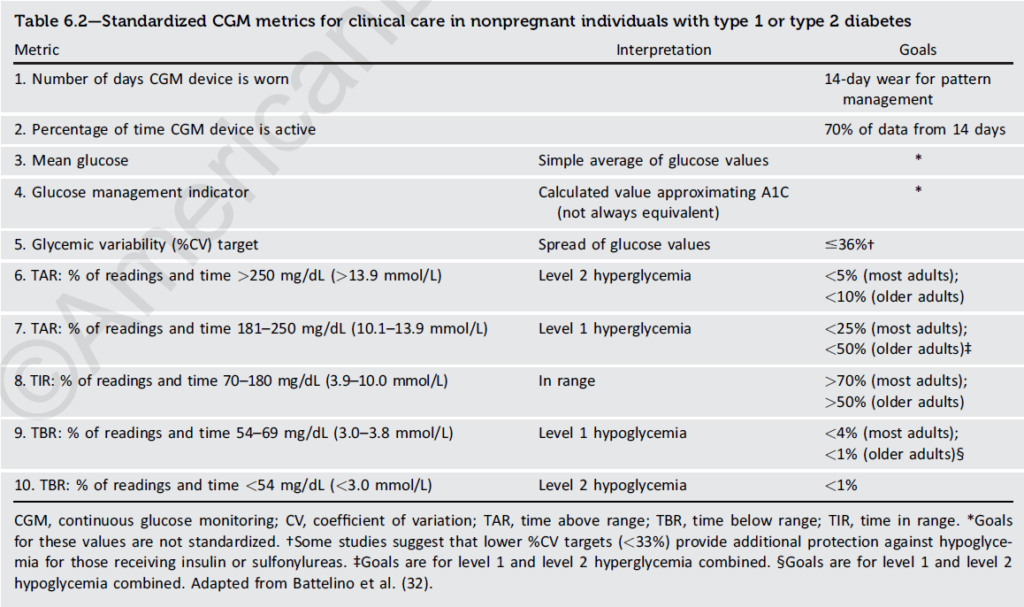
(圖片來源:ADA-Standards of Care in Diabetes—2024)
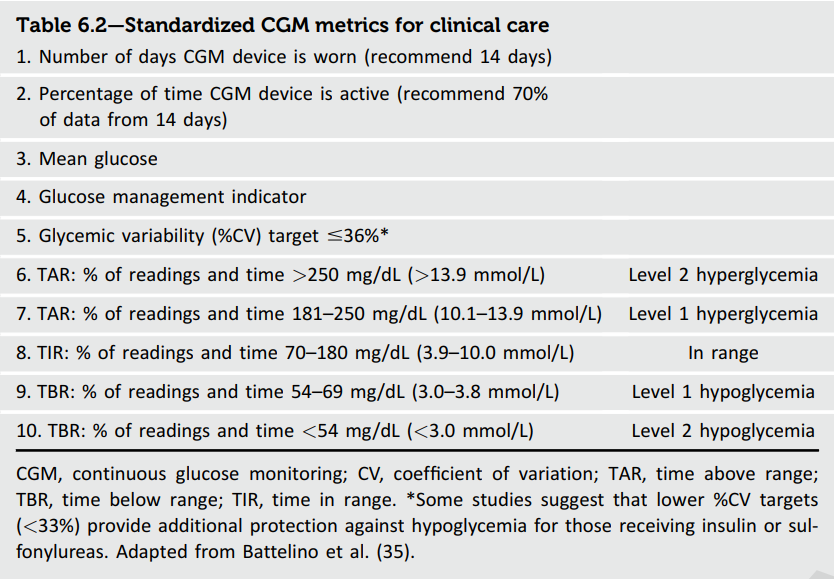
(圖片來源:ADA-Standards of Care in Diabetes—2023)
- 討論了作為A1C替代品的血清糖化蛋白測試(serum glycated protein assays)的益處和局限性。
Fructosamine and glycated albumin are alternative measures of glycemia that are approved for clinical use for monitoring glycemic status in people with diabetes. Fructosamine reflects total glycated serum proteins (mostly albumin). Glycated albumin assays reflect the proportion of total albumin that is glycated. Due to the turnover rate of serum protein, fructosamine and glycated albumin reflect glycemia over the past 2–4 weeks, a shorter-term time frame than that of A1C. Fructosamine and glycated albumin are highly correlated in people with diabetes, and the performance of modern assays is typically excellent.
- 明定哪些臨床情境下減弱糖尿病藥物是適當的。
Deintensify hypoglycemia-causing medications (insulin, sulfonylureas, or meglitinides), or switch to a medication class with lower hypoglycemia risk, for individuals who are at high risk for hypoglycemia, within individualized glycemic goals.
- 更新了表6.5,提供低血糖風險因子的摘要。
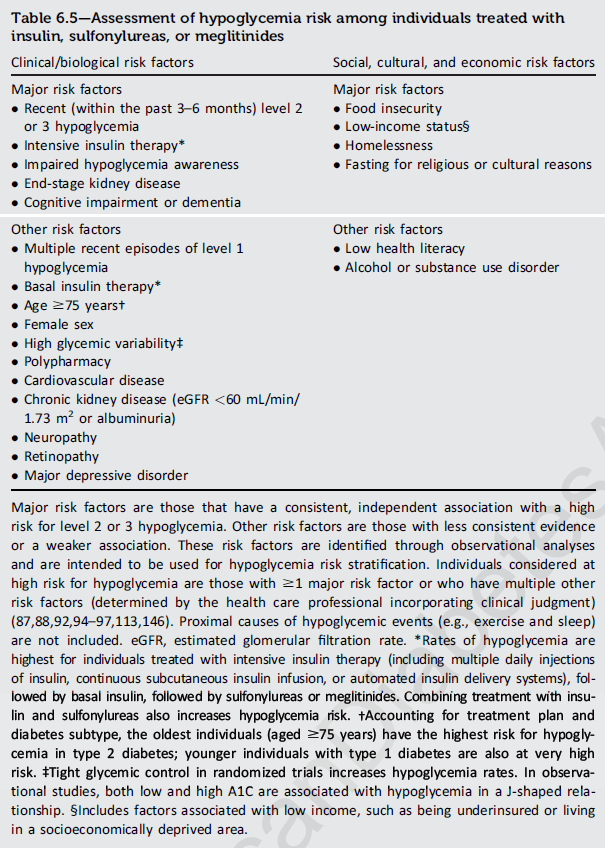
(圖片來源:ADA-Standards of Care in Diabetes—2024)
(圖片來源:ADA-Standards of Care in Diabetes—2023)
- 增加連續血糖監測(CGM)用於低血糖預防的好處。
CGM can be a valuable tool for detecting and preventing hypoglycemia in many individuals with diabetes, and it is recommended for insulin-treated individuals, especially those using multiple daily insulin injections or continuous subcutaneous insulin infusion.
- 新增升血糖產品成本比較表(Table 6.6)。
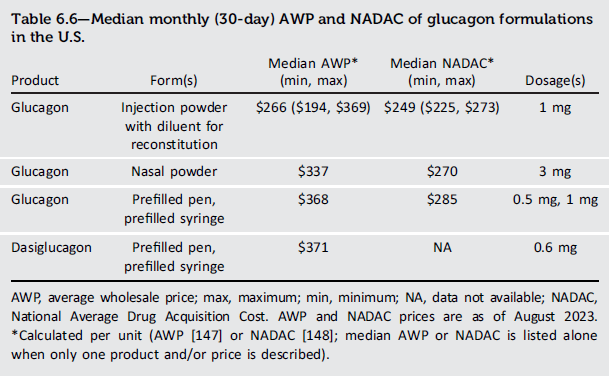
(圖片來源:ADA-Standards of Care in Diabetes—2024)
第七章修訂內容(糖尿病技術)
- 強調需要在第1型糖尿病診斷甚至更早開始使用CGM,以利早期達到血糖控制目標。支持第1型糖尿病個體在診斷時甚至更早開始使用胰島素幫浦和/或AID系統。
Initiation of continuous glucose monitoring (CGM) should be offered to people with type 1 diabetes early in the disease, even at time of diagnosis.
- 擴展了關於CGM系統的內容,包括更新已獲批准與AID系統集成的系統,以及CGM在使用非密集胰島素治療和/或未使用胰島素治療的2型糖尿病患者中的益處。
The text on CGM systems was expanded to include updates on systems that are cleared for integration with AID systems and to include the benefits of CGM use in type 2 diabetes for those using nonintensive insulin therapy and/or not using insulin therapy.
- 更新干擾CGM裝置準確性的藥物。
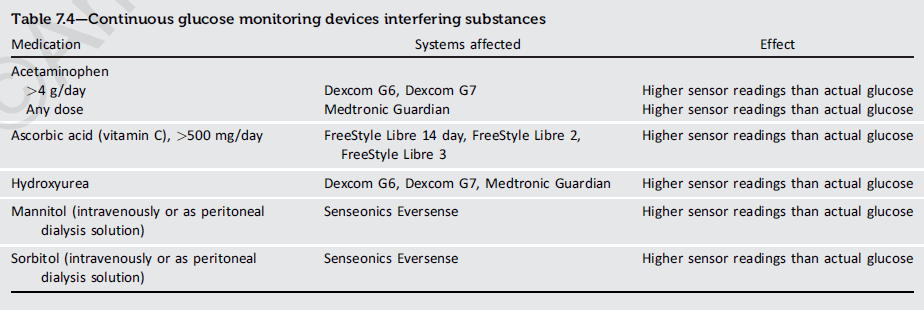
(圖片來源:ADA-Standards of Care in Diabetes—2024)
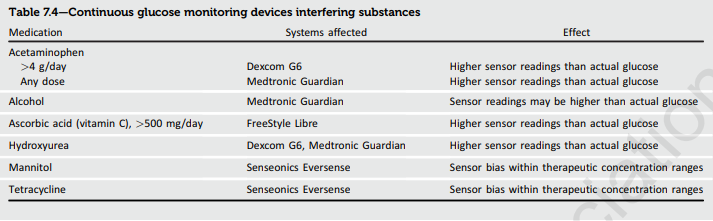
(圖片來源:ADA-Standards of Care in Diabetes—2023)
- 強調在臨床適當的情況下,患者在住院期間應繼續使用個人CGM裝置。
In people with diabetes using personal CGM, the use of CGM should be continued when clinically appropriate during hospitalization, with confirmatory point-of-care glucose measurements for insulin dosing and hypoglycemia assessment and treatment under an institutional protocol.
第八章修訂內容(肥胖和體重管理)
調整章節用詞,更以人為中心,強調體重管理在糖尿病患者整體治療中的重要性。例如:“obese person” 修改為 “person with obesity”。
- 擴展BMI外的額外人體計量測量(即,腰圍、腰臀比和/或腰高比),以鼓勵對體脂肪量和分佈進行個體化評估。
BMI should not be relied on as a sole diagnostic and staging tool. BMI is especially prone to misclassification in individuals who are very muscular or frail, as well as in populations with different body composition and cardiometabolic risk.
A diagnosis of obesity should be made based on an overall assessment of the individual’s adipose tissue mass (BMI can be used as a general guidance), distribution (using other anthropometric measurements like waist circumference, waist-to-hip circumference ratio, or waist-to-height ratio), or function and, importantly, the presence of associated health or well-being consequences: metabolic, physical, or psychological/well-being.
- 增加建議,包括Glucagon-like peptide-1(GLP-1)receptor agonist 或具有更大減重效果的gastric inhibitory polypeptide(GIP)和GLP-1受體促效劑作為糖尿病患者肥胖管理的首選藥物療法。
- 更新表8.1中幾種肥胖藥物的最新FDA批准和價格變化。
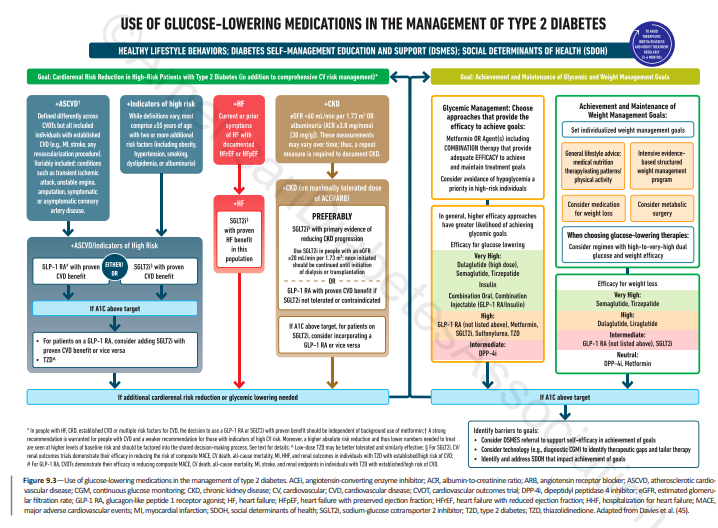
第九章修訂內容(血糖治療的藥物方法)
- 更新建議,對大多數成年第1型糖尿病患者而言,為了減少低血糖風險,優先選擇胰島素類似物或吸入胰島素而非注射人類胰島素。
- 建議早期對成年第1型糖尿病患者使用CGM,另指出應考慮為成年第1型糖尿病患者使用AID系統。
Intensive insulin management using a version of CSII and CGM should be considered in individuals with type 1 diabetes whenever feasible. AID systems are preferred and should be considered for individuals with type 1 diabetes who are capable of using the device safely (either by themselves or with a caregiver) to improve time in range and reduce A1C and hypoglycemia.
- 增加建議,為使用胰島素或高風險低血糖患者開立處方葡萄糖。
Glucagon should be prescribed for all individuals taking insulin or at high risk for hypoglycemia.
- 增加建議,藥物治療應同時解決成年第2型糖尿病患者的血糖和體重問題,即使他們沒有心血管疾病和/或腎病。
- 增加建議,建議考慮為未達到個體化血糖目標的成年2型糖尿病患者添加其他降血糖藥物。
- 增加建議,強調治療加強和方法組合對於成年2型糖尿病患者的體重管理及其與血糖管理目標的一致性的重要性。
- 更新建議,指出在成年2型糖尿病患者中,優先選擇同時降低心血管和腎病風險的血糖管理藥物,尤其是那些已確立/高風險動脈粥樣硬化性心血管疾病、心衰和/或慢性腎病的患者。
In adults with type 2 diabetes without cardiovascular and/or kidney disease, pharmacologic agents should address both the individualized glycemic and weight goals.
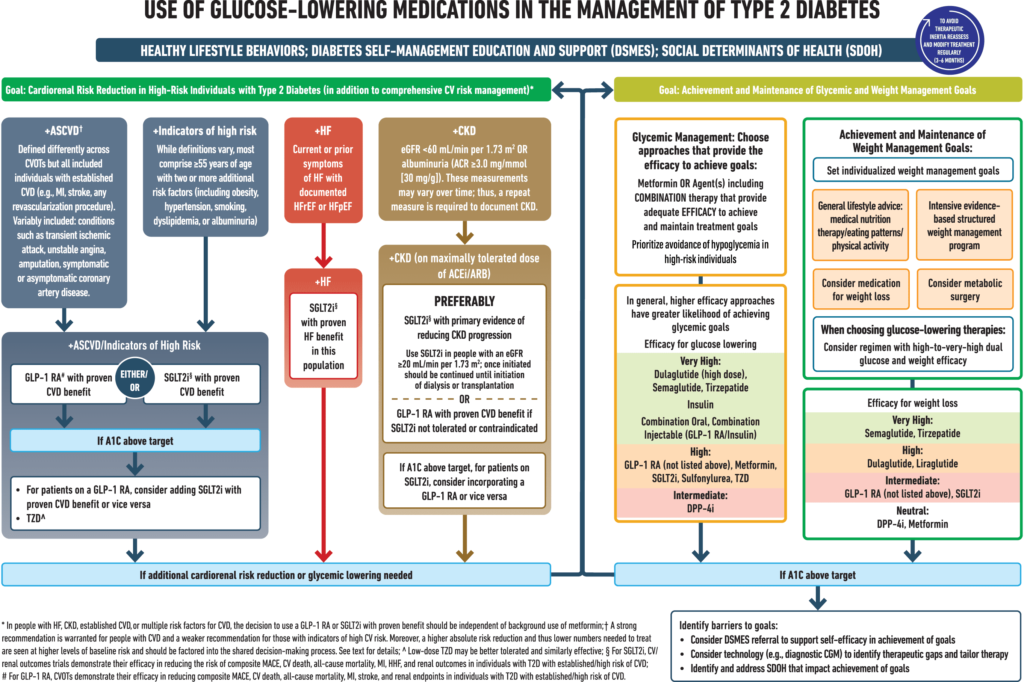
(圖片來源:ADA-Standards of Care in Diabetes—2024)
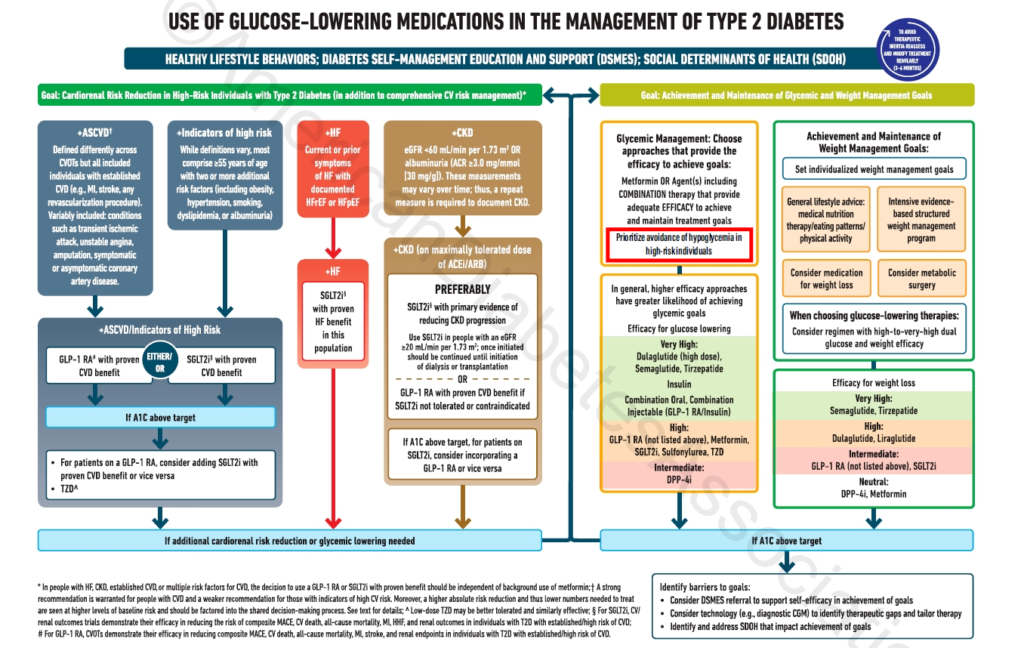
僅有紅框處更新
(圖片來源:ADA-Standards of Care in Diabetes—2024)
(圖片來源:ADA-Standards of Care in Diabetes—2023)
- 對於有心衰的成年2型糖尿病患者,增加了建議9.19,建議使用SGLT2抑制劑進行血糖管理,並預防心衰住院治療。
- 更新建議,雙重GIP和GLP-1受體激動劑作為更強血糖管理效果的額外選擇,優先於胰島素。
In adults with type 2 diabetes, a GLP-1 RA, including a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 RA, is preferred to insulin.
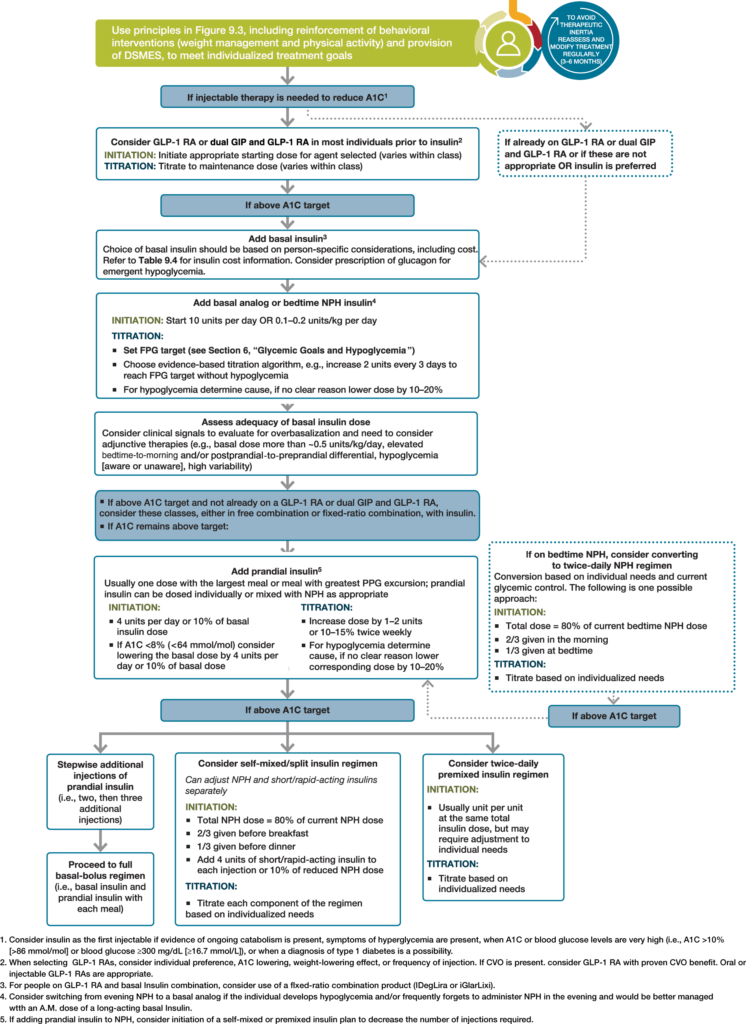
(圖片來源:ADA-Standards of Care in Diabetes—2024)
- 更新表9.2,包括關於腸阻塞潛在風險(皮下注射的semaglutide),以及有胃輕癱病史的個體不建議使用雙重GIP和GLP-1受體激動劑治療。
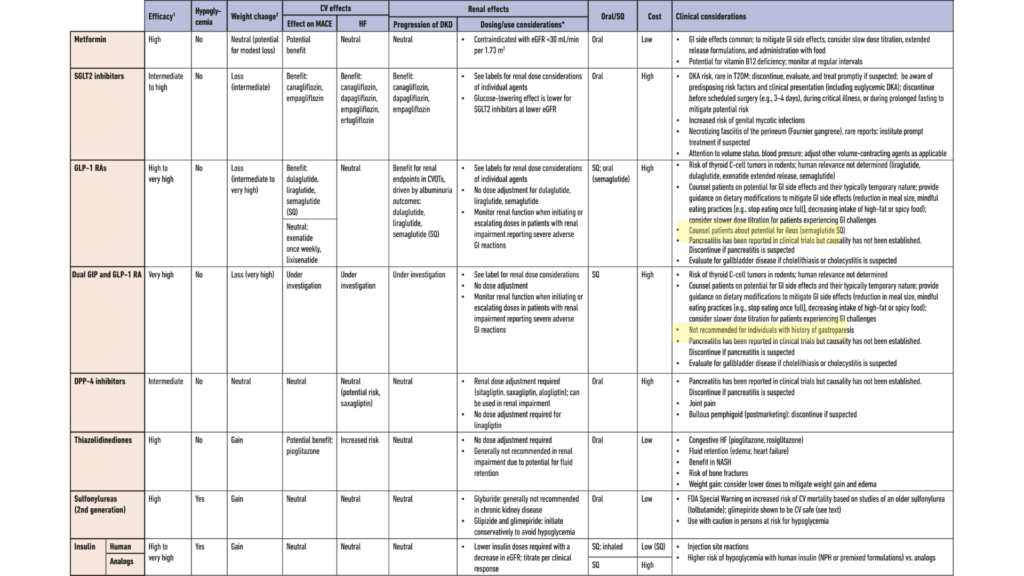
螢光筆處為2024年新增項目。
(圖片來源:ADA-Standards of Care in Diabetes—2024)
第十章修訂內容(心血管疾病和風險管理)
- 建議在開始使用血管緊張素轉化酶(ACE)抑制劑、血管緊張素受體阻滯劑、礦質皮質激素受體拮抗劑或利尿劑治療後的7至14天內監測血清肌酐/估計腎小球過濾率和鉀。
- 增加了建議10.24,包括對不耐受他汀治療且未建立心血管疾病的糖尿病患者進行bempedoic acid治療。此外,建議10.28b推薦bempedoic acid或蛋白酶轉化酶/凱克辛型9(PCSK9)抑制劑治療,與單克隆抗體治療或inclisiran siRNA作為替代的降膽固醇治療。新增了“他汀耐受性”小節,以擴展這些更新。
- 建議在糖尿病患者發生急性冠狀動脈綜合徵或缺血性中風/短暫性腦缺血發作後,由包括心血管或神經專家的跨專業團隊決定使用雙重抗血小板療法的治療長度。
- 增加建議,包括篩查糖尿病成人的無症狀心衰竭,透過測量利鈉肽水平以預防或延緩心衰竭的發展。
Adults with diabetes are at increased risk for the development of asymptomatic cardiac structural or functional abnormalities (stage B heart failure) or symptomatic (stage C) heart failure. Consider screening adults with diabetes by measuring a natriuretic peptide (B-type natriuretic peptide [BNP] or N-terminal pro-BNP [NT-proBNP]) to facilitate prevention of stage C heart failure.
In asymptomatic individuals with diabetes and abnormal natriuretic peptide levels, echocardiography is recommended to identify stage B heart failure.
- 修改了建議10.40,包括在無症狀的糖尿病患者中進行周邊動脈疾病篩查,使用踝臂指數測試,尤其是年齡≥50歲、任何部位的微血管疾病、足部並發症或任何由糖尿病引起的器官損傷的患者。對於糖尿病患者超過10年以上,應考慮進行周邊動脈疾病篩查。
- 更新了建議10.42a,建議對於有心衰且心室收縮功能保留或降低的糖尿病患者,使用SGLT2抑制劑或SGLT1/2抑制劑,以減少心衰惡化和心血管死亡的風險。
In people with type 2 diabetes and established heart failure with either preserved or reduced ejection fraction, an SGLT2 inhibitor (including SGLT1/2 inhibitor) with proven benefit in this patient population is recommended to reduce the risk of worsening heart failure and cardiovascular death.
- 增加了建議,建議對於使用SGLT抑制劑治療的第1型糖尿病、易罹患酮症的第2型糖尿病患者,以及生酮飲食的人,包括對酮症酸中毒的風險和徵兆、管理方法和檢測工具的教育。
- 修改了圖10.2,以反映非孕婦糖尿病患者確認高血壓的初始血壓值和治療建議的變化。
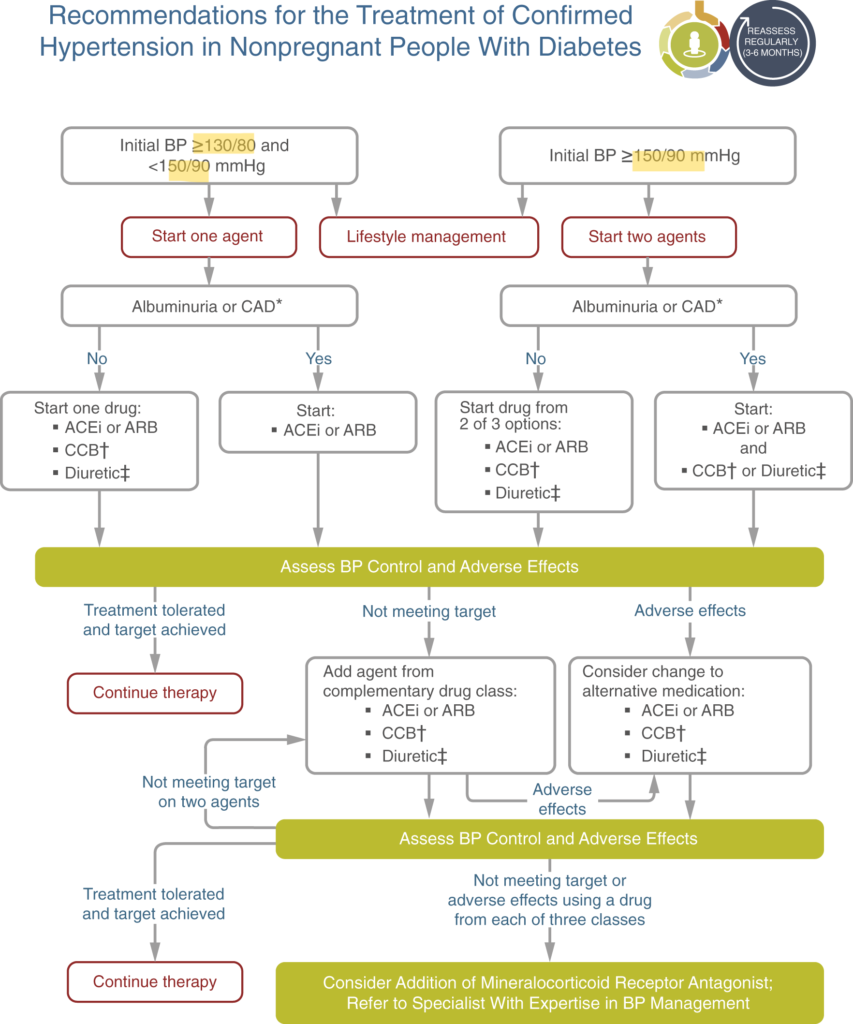
螢光筆處為2024年修改項目。
(圖片來源:ADA-Standards of Care in Diabetes—2024)
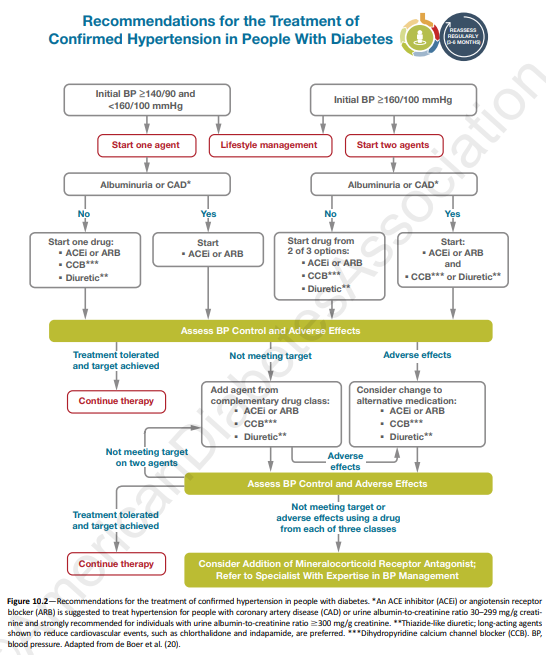
(圖片來源:ADA-Standards of Care in Diabetes—2023)
第十一章修訂內容(慢性腎病和風險管理)
- 更新了建議11.4a,強調ACEIs及ARBs在預防腎病進展和減少心血管事件中的作用。
In nonpregnant people with diabetes and hypertension, either an ACE inhibitor or an angiotensin receptor blocker (ARB) is recommended for those with moderately increased albuminuria (UACR 30–299 mg/g creatinine) and is strongly recommended for those with severely increased albuminuria (UACR ≥300 mg/g creatinine) and/or eGFR <60 mL/min/1.73 m2 to prevent the progression of kidney disease and reduce cardiovascular events.
- 更新了圖11.1,整理慢性腎病進展、訪視頻率,以及根據腎小球過濾率和白蛋白尿症向腎臟科醫師轉介的情況。
- 新增了圖11.2,整理了改善糖尿病和慢性腎病患者治療結果的方法。
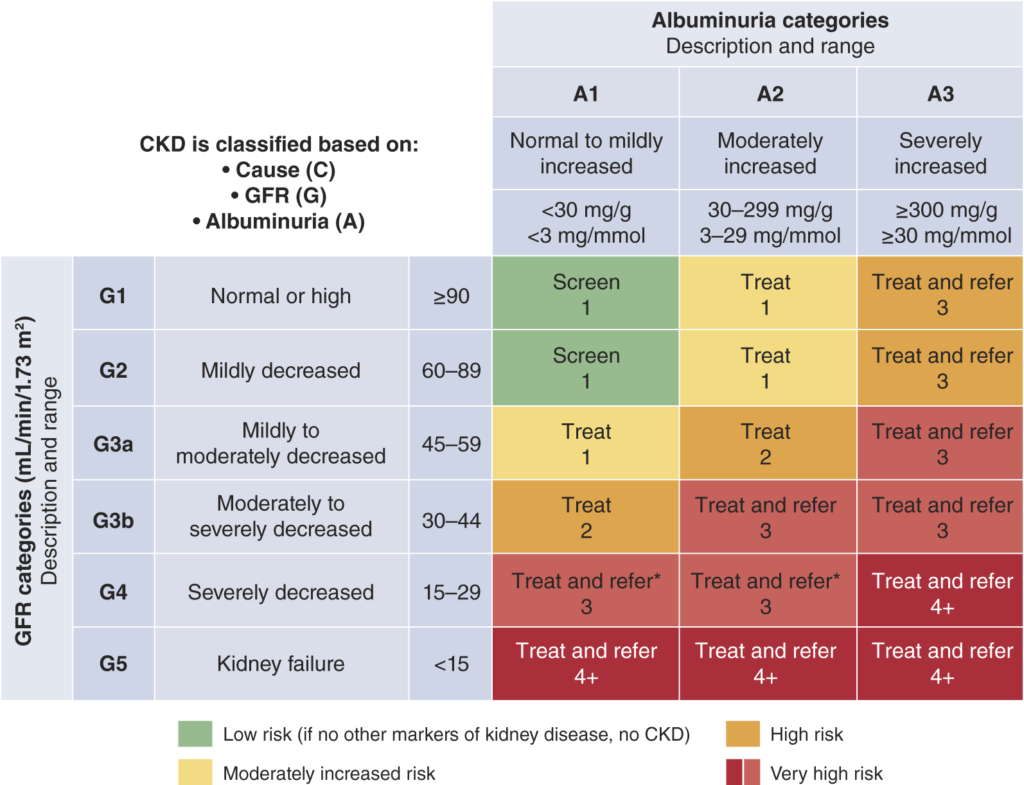
(圖片來源:ADA-Standards of Care in Diabetes—2024)
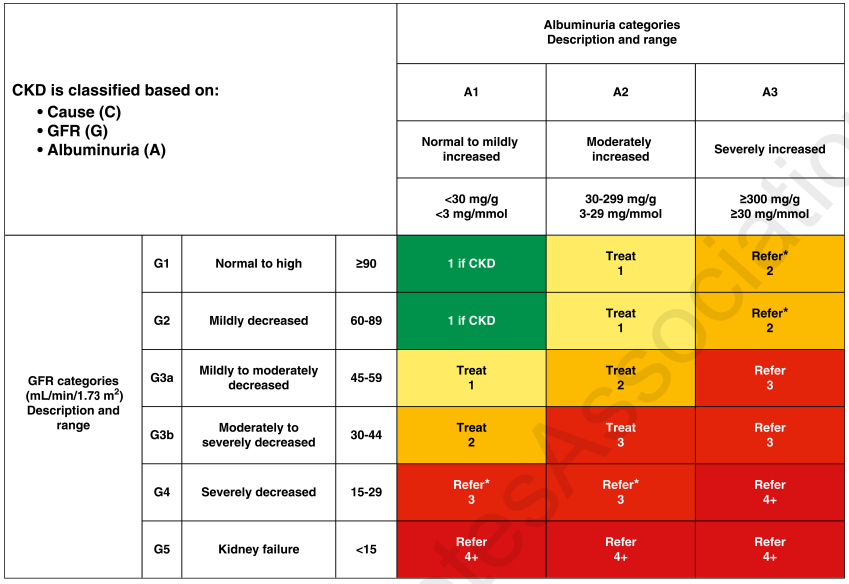
(圖片來源:ADA-Standards of Care in Diabetes—2023)
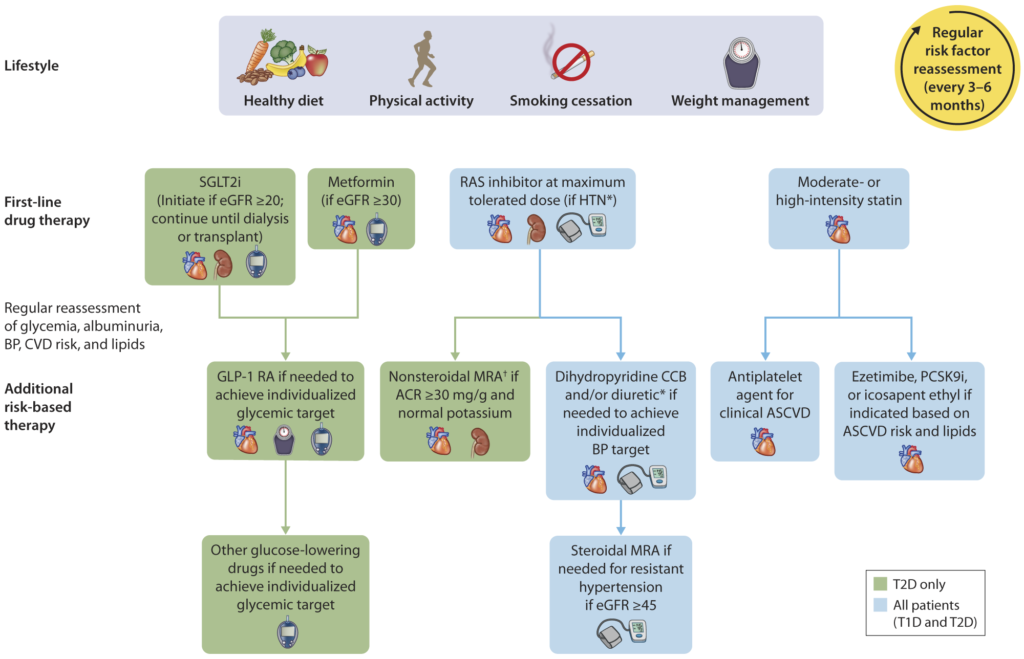
(圖片來源:ADA-Standards of Care in Diabetes—2024)
第十二章修訂內容(視網膜病變、神經病變和足部護理)
- 更新了建議12.6,指出應用FDA批准的人工智能算法,並更新了內容,提供批准的人工智能算法的詳細信息和臨床試驗。
Programs that use retinal photography with remote reading or the use of U.S. Food and Drug Administration–approved artificial intelligence algorithms to improve access to diabetic retinopathy screening are appropriate screening strategies for diabetic retinopathy. Such programs need to provide pathways for timely referral for a comprehensive eye examination when indicated.
- 增加了建議12.15和12.16,處理因糖尿病導致的視力喪失,並擴展了內容,討論視力喪失的並發症和評估與康復的重要性。
People who experience vision loss from diabetes should be counseled on the availability and scope of vision rehabilitation care and provided, or referred for, a comprehensive evaluation of their visual impairment by a practitioner experienced in vision rehabilitation.
People with vision loss from diabetes should receive educational materials and resources for eye care support in addition to self-management education (e.g., glycemic management and hypoglycemia awareness).
- 在“足部護理”小節中,更新了建議12.27,包括在篩查周邊動脈疾病時使用足趾壓力。
Initial screening for peripheral arterial disease (PAD) should include assessment of lower-extremity pulses, capillary refill time, rubor on dependency, pallor on elevation, and venous filling time. Individuals with a history of leg fatigue, claudication, and rest pain relieved with dependency or decreased or absent pedal pulses should be referred for ankle-brachial index with toe pressures and for further vascular assessment as appropriate.
第十三章修訂內容(老年人)
- 更新了建議13.16a至13.16d,強調了減少治療強度的需要,特別是對於會引起低血糖的藥物。這些建議還建議轉換到低血糖風險較低的降糖藥物類別,以達到個體化的血糖目標。此外,對於患有動脈粥樣硬化性心血管疾病、心衰竭和/或慢性腎病等其他合併症的老年糖尿病患者的治療計劃應包括降低心腎風險的藥物,無論血糖水平如何。
In older adults with diabetes, deintensify hypoglycemia-causing medications (e.g., insulin, sulfonylureas, or meglitinides) or switch to a medication class with low hypoglycemia risk for individuals who are at high risk for hypoglycemia, using individualized glycemic goals.
In older adults with diabetes, deintensify diabetes medications for individuals for whom the harms and/or burdens of treatment may be greater than the benefits, within individualized glycemic goals.
Simplification of complex treatment plans (especially insulin) is recommended to reduce the risk of hypoglycemia and polypharmacy and decrease the treatment burden if it can be achieved using the individualized glycemic goals.
In older adults with type 2 diabetes and established or high risk of atherosclerotic cardiovascular disease, heart failure, and/or chronic kidney disease, the treatment plan should include agents that reduce cardiorenal risk, irrespective of glycemia.
第十四章修訂內容(兒童和青少年)
- 增加了建議14.4,指出根據膳食成分調整胰島素劑量的需要。
Meal composition impacts postprandial glucose excursions. Education on the impact of high-fat and high-protein meals and the adjustment of insulin dosing is necessary.
- 修改了建議14.53,建議為超重和肥胖的2型糖尿病青少年推薦“至少”減少7-10%的超重體重。
Youth with overweight/obesity and type 2 diabetes and their families should be provided with developmentally and culturally appropriate comprehensive lifestyle programs that are integrated with diabetes management to achieve at least a 7–10% decrease in excess weight.
- 更新了建議14.68和14.70,包括在開始和/或加強胰島素治療計劃以進行血糖管理之前,考慮使用empagliflozin,並更新了圖14.1以包括empagliflozin。
If glycemic goals are no longer met with metformin (with or without long-acting insulin), glucagon-like peptide 1 (GLP-1) receptor agonist therapy and/or empagliflozin should be considered in children 10 years of age or older.
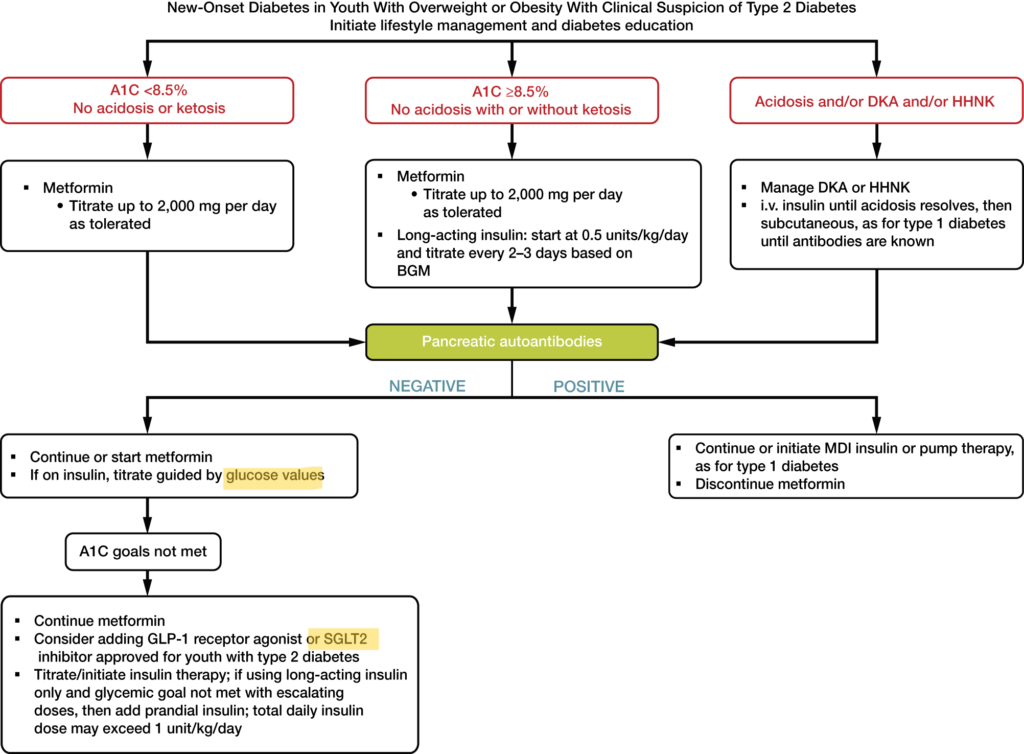
螢光筆處為2024年修改項目。
(圖片來源:ADA-Standards of Care in Diabetes—2024)
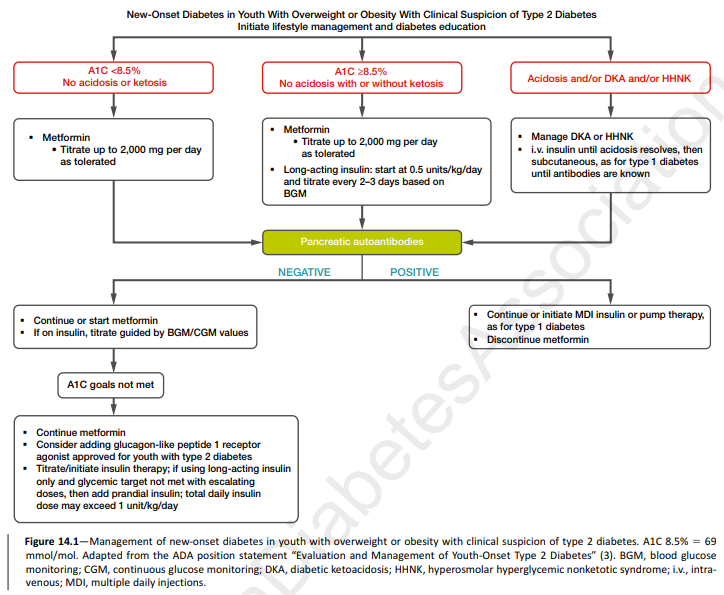
(圖片來源:ADA-Standards of Care in Diabetes—2023)
- 增加了建議14.69,建議考慮藥物服用行為和藥物對體重的影響,適用於超重或肥胖的第2型糖尿病青少年。
- 更新了建議14.78,以澄清根據年齡調整患有腎病的蛋白攝入量。
Protein intake should be at the recommended daily allowance of 0.85–1.2 g/kg/day (according to age).
- “兒童糖尿病中的物質使用”小節中包括建議14.106和14.107,以阻止青少年開始吸菸(菸草和電子菸)並鼓勵戒菸。討論青少年糖尿病患者吸菸和接觸二手菸的不良健康影響。
第十五章修訂內容(懷孕期間的糖尿病管理)
- 在“懷孕期間的血糖目標”小節中,修改了建議15.7,強調所有懷孕的糖尿病患者應監測空腹、餐前和餐後血糖水平,並更新了建議15.10,以包括對懷孕的第1型糖尿病患者使用CGM。
Fasting, preprandial, and postprandial blood glucose monitoring are recommended in individuals with diabetes in pregnancy to achieve optimal glucose levels. Glucose goals are fasting plasma glucose <95 mg/dL (<5.3 mmol/L) and either 1-h postprandial glucose <140 mg/dL (<7.8 mmol/L) or 2-h postprandial glucose <120 mg/dL (<6.7 mmol/L).
CGM is recommended in pregnancies associated with type 1 diabetes. When used in addition to blood glucose monitoring, achieving traditional pre- and postprandial goals, real-time CGM can reduce the risk for large-for-gestational age infants and neonatal hypoglycemia in pregnancy complicated by type 1 diabetes.
- 更新了建議15.15,指出metformin和glyburide單獨或聯合使用不應作為治療懷孕期高血糖的一線藥物。
Insulin is the preferred medication for treating hyperglycemia in GDM. Metformin and glyburide, individually or in combination, should not be used as first-line agents, as both cross the placenta to the fetus. Other oral and noninsulin injectable glucose-lowering medications lack long-term safety data.
- 更新了建議15.27,鼓勵所有糖尿病患者於產後哺乳。
Breastfeeding efforts are recommended for all individuals with diabetes. Breastfeeding is recommended for individuals with a history of GDM for multiple benefits, including a reduced risk for type 2 diabetes later in life.
- “產後護理”小節已更新,解釋了對於具有糖尿病前期或有妊娠期糖尿病(GDM)病史且有生育潛力的個體,需要進行孕前評估。
第十六章修訂內容(醫院中的糖尿病護理)
- 更新了建議16.4,建議當患者血糖持續高於180 mg/dL(10.0 mmol/L)以上,應開始或加強胰島素或其他降血糖治療。
Insulin and/or other therapies should be initiated or intensified for treatment of persistent hyperglycemia starting at a threshold of ≥180 mg/dL (≥10.0 mmol/L) (confirmed on two occasions within 24 h) for noncritically ill (non-ICU) individuals.
- 增加了建議16.5a,界定了大多數嚴重病患(most critically ill individuals)的血糖目標(目標血糖範圍為140-180 mg/dL [7.8-10.0 mmol/L]),並更新了建議16.5b,建議對選定的嚴重患者(selected critically ill individuals)實施更嚴格的目標(110-140 mg/dL [6.1-7.8 mmol/L])。
Once therapy is initiated, a glycemic goal of 140–180 mg/dL (7.8–10.0 mmol/L) is recommended for most critically ill (ICU) individuals with hyperglycemia.
More stringent glycemic goals, such as 110–140 mg/dL (6.1–7.8 mmol/L), may be appropriate for selected critically ill individuals and are acceptable if they can be achieved without significant hypoglycemia.
- 增加了建議16.6和16.7,分別指出在臨床適當的情況下,在住院環境中繼續使用個人CGM裝置和AID系統與CGM結合使用,並且如果有可用資源和培訓,且依據醫療機構協議,使用point-of-care血糖測量進行胰島素劑量決策和低血糖評估。此外,敘述還擴展了在整個住院期間實現血糖目標的個性化方法。
In people with diabetes using a personal continuous glucose monitoring (CGM) device, the use of CGM should be continued during hospitalization if clinically appropriate, with confirmatory point-of-care (POC) glucose measurements for insulin dosing decisions and hypoglycemia assessment, if resources and training are available, and according to an institutional protocol.
For people with diabetes using an automated insulin delivery (AID) system along with CGM, the use of AID and CGM should be continued during hospitalization if clinically appropriate, with confirmatory POC blood glucose measurements for insulin dosing decisions and hypoglycemia assessment, if resources and training are available, and according to an institutional protocol.
- 在“手術期照護”小節中,增加了關於GLP-1受體促效劑在手術期照護的安全使用的聲明。
There are little data on the safe use and/or influence of GLP-1 receptor agonists on glycemia and delayed gastric emptying in the perioperative period.
- 增加了建議16.11,指出對於住院治療心衰竭的第2型糖尿病患者使用SGLT2抑制劑,並應在從急性病情恢復後繼續使用SGLT2抑制劑,如果沒有禁忌症的話。
For people with type 2 diabetes hospitalized with heart failure, it is recommended that use of a sodium–glucose cotransporter 2 inhibitor be initiated or continued during hospitalization and upon discharge, if there are no contraindications and after recovery from the acute illness.
第十七章修訂內容(糖尿病倡議)
- 更新兒童保育和社區環境中的糖尿病兒童護理倡議聲明。
以上為2024年美國ADA發布新版糖尿病臨床照護指引更新內容之整理,部分細微更動礙於篇幅有進行刪減,完整更新內容原文連結:Summary of Revisions: Standards of Care in Diabetes—2024 。